What do my Prolaris results mean?
The Prolaris® test provides an analysis of your individual tumor aggressiveness as well as a clinically validated prostate cancer-specific mortality risk.
Two patients with the same PSA and Gleason scores may have a very different estimate of mortality risk when their Prolaris Score is included in their evaluation. Since cancer is the uncontrolled rapid growth of abnormal cells, an aggressive prostate tumor carries the potential risk of growing and spreading rapidly to other parts of your body.
The Prolaris Score is calculated by directly measuring the biology of the tumor and how fast the cells in your tumor or dividing. Since you have already had a biopsy which determined that you have prostate cancer, that tissue sample can also be used to determine your Prolaris Score. And, because every individual’s prostate cancer is different, the result of your Prolaris test is unique to you.
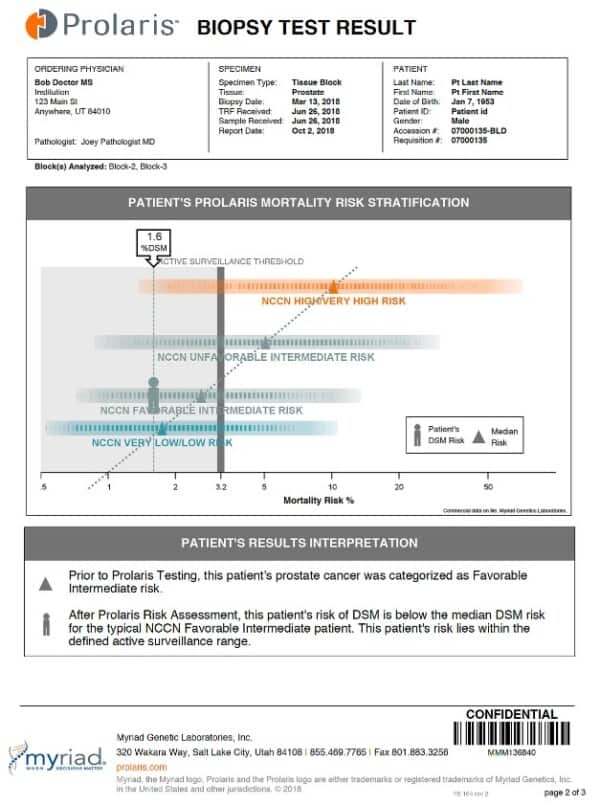
Patient Sample Report:
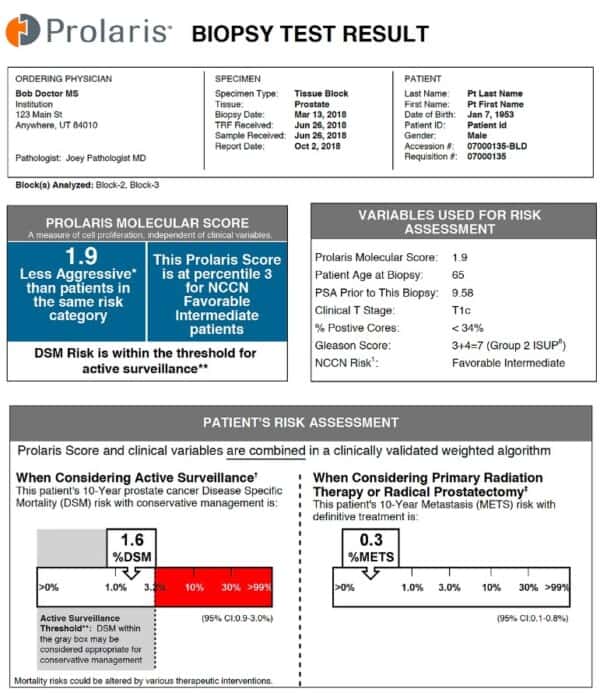
The Prolaris Molecular Score:
The Prolaris Molecular Score reveals the aggressiveness of the individual’s prostate cancer while the relative risk shows how a patient’s score compares to the average score in their National Comprehensive Cancer Network (NCCN) risk category. The majority of Prolaris Molecular Scores will fall between 0 and 10, with a higher score indicating a more aggressive cancer. For every 1 unit increase in the Prolaris Molecular Score, the patient’s risk doubles.
Clinical Variables and the Prolaris Molecular Score:
When Considering Active Surveillance:
10 year risk of cancer spread after radiation or prostate removal surgery (prostatectomy):