Knowing your risk of developing prostate cancer can help you enjoy a longer and healthier life.
After skin cancer, prostate cancer is the most common form of cancer in men. It’s also the second leading cause of cancer death in men.
Fortunately, however, most men will not die from prostate cancer because it’s a highly treatable disease when diagnosed in early stages.
Unfortunately, prostate cancer in its earliest stages has no symptoms or warning signs.
When prostate cancer is confined to the prostate or nearby lymph nodes, men have nearly a 100% 5-year survival rate. When prostate cancer spreads to other parts of the body, that drops to 34%, according to the National Cancer Institute.
That’s why it’s important to know your risk and know when and how to get screened.
So how can you determine your risk of developing prostate cancer? Age, race, and genetics are the most important factors influencing your risk:
- Age: By far, this is the greatest risk factor. Roughly 60% of prostate cancer cases are found in men who are ages 65 and older.
- Family History: Men who have a father or brother with prostate cancer are twice as likely to develop prostate cancer than men who don’t have familial prostate cancer. Men who have several family members with prostate cancer are at greater risk.
- Genetic Mutations : Genetic mutations are changes in the DNA sequence in genes that can be inherited (hereditary cancer) or may occur during a person’s lifetime. Genetic mutations that are inherited, such as mutations to the BRCA1, BRCA2, CHEK2, ATM, PALB2, RAD51D, RNASEL, HOXB13 genes and others may account for up to 10% of prostate cancers. Men with immediate family members with prostate cancer and those whose have a family history of breast, colorectal, ovarian, and pancreatic may benefit from testing for genetic mutations.
- Race: Black men are 70% more likely to develop prostate cancer than White men. Latino, Asian American, and Hispanic men are at lower risk of developing prostate cancer than non-Hispanic White men. While not fully understood, access to care and genetics may have a role in race contributing to a man’s risk.
Early Detection of Prostate Cancer
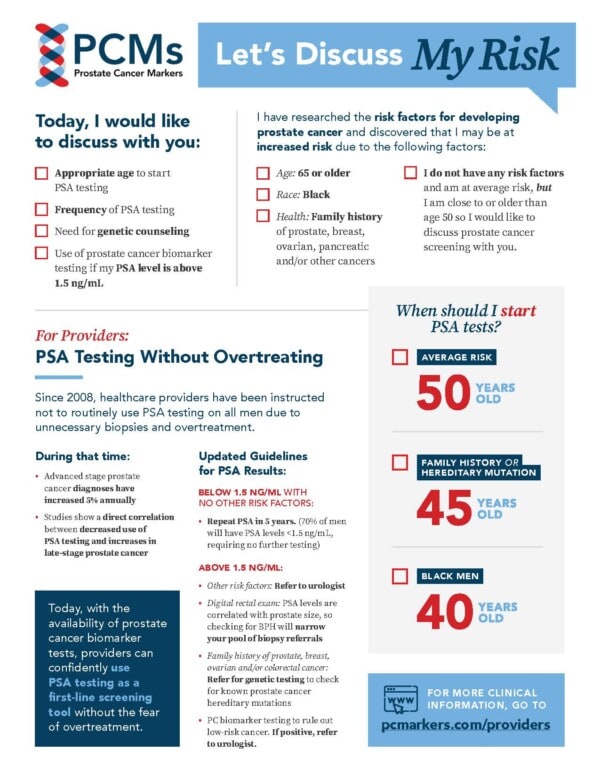
Men who do not have any known factors putting them at higher-than-average risk for developing prostate cancer should obtain a screening PSA blood test at age 50. If the result of that test is less than 1.5 ng/mL, they probably won’t need another test for 5 years but should consult their primary care providers.
Men who have one or more factors that put them at higher- than-average risk for developing prostate cancer should start prostate cancer screening earlier and more often to ensure that any cancer is detected at its earliest and most treatable stages. Recommendations are:
- Men with a family history or known genetic mutation should start screening at age 45 or earlier.
- Black men should consider prostate cancer screening at age 40.
The PSA test is the best starting point. It is a simple blood test that can be done as part of a normal doctor’s visit. However, it is just a basic test that indicates something might be amiss. If your result is above 1.5 ng/mL, there is no need to worry. Your healthcare provider will next run some additional tests, including prostate cancer biomarkers that can help determine if your elevated levels are due to a non-cancerous condition or a low-level non-aggressive form of cancer that can be watched.
Talk to Your Primary Care Provider
Genetic Tests Associated With Prostate Cancer
While some men have a family history of cancer that puts them at higher risk, others may have inherited a genetic mutation that puts them at an increased risk of developing prostate cancer. This is called hereditary prostate cancer and accounts for up to 10% of all cases, according to the American Cancer Society.
Genetic tests evaluate your genes to identify whether you carry any genetic mutations associated with prostate cancer. If you test positive, it does not mean you will develop prostate cancer just that you are at higher risk than men without these mutations. Because you are at higher risk, you should be diligent about screenings so that if cancer develops, it can be diagnosed and treated early.
These are genetic tests that look for genetic mutations associated with prostate cancer:

ProstateNext
The ProstateNext genetic test analyzes 14 genes, including the BRCA1 and BRCA2 genes, to determine a man’s risk of developing hereditary prostate cancer.

Myriad MyRisk
The Myriad MyRisk Hereditary Cancer test can be effective in identifying a man's elevated risk for eight hereditary cancers, including prostate cancer.
%s
FAQs about Risk
Below is an initial list of frequently asked questions about prostate cancer risk, PSA screening and PCM tests relevant to this topic.
No, in fact less than 30% of men with a PSA level >4.0 ng/mL will be diagnosed with cancer. Unfortunately, the PSA test cannot differentiate between cancer and non-cancerous conditions like an infection (prostatitis), a urinary tract infection (UTI), an enlarged prostate (benign prostatic hyperplasia), or other non-cancerous conditions. Certain types of vigorous exercise, such as cycling, and sexual intercourse can stimulate the prostate and cause PSA levels to rise so men should abstain from both at least 48 hours prior to a PSA test. Regular use of certain medications including statins, NSAIDs, and thiazide diuretics have been shown to cause a decrease in PSA levels, so men should alert their physicians if taking these medications. Conversely, other medications, such as testosterone, can raise PSA levels. Having a digital rectal exam (DRE) prior to a PSA blood test can also momentarily raise PSA levels, which is why the PSA test should be conducted first.
Because the PSA test is a simple, inexpensive blood test, it’s a great first step in identifying men who may benefit from additional testing including prostate cancer biomarkers, which can provide more insights about what is causing elevated PSA levels.
The PSA test cannot differentiate between prostate cancer and non-cancerous (benign) conditions, such as benign prostatic hyperplasia (BPH). Men who receive a PSA level above 1.5 ng/ML should discuss additional biomarker testing with their healthcare providers prior to considering a prostate biopsy.
Prostate cancer biomarkers (PCMs) are molecules found in blood, tissue, or body fluids. PCMs are revolutionary new, non-invasive diagnostic tests that may help your healthcare provider decide if your prostate cancer is in fact low risk, if something more aggressive may be lurking in your prostate, or if there are hot spots in the prostate that may need to be re-evaluated upon biopsy. PCMs also can help you and your healthcare provider determine the most appropriate treatment for your cancer.
If you have had a prostatectomy and are at risk of your cancer spreading or recurring, the following PCMs could be helpful:
If your physician has recommended radiation to treat your prostate cancer, the following tests can help inform your treatment plan. Or, if you have had radiation and underwent another biopsy, these tissue-based tests could help you and your healthcare provider assess whether you may need additional treatment down the line. However, many radiation oncologists may want to wait until your PSA rises +2ng/ml above the lowest point after your radiation to see if further biopsies or treatment are necessary.
Although there are many factors that contribute to your healthcare provider’s decision to conduct a prostate biopsy, there are several urinary and blood based PCMs that may help guide you and your physician through the decision of conducting a prostate biopsy. These include:
Genetic tests also may be worth considering if you have a family history of prostate cancer, breast cancer, ovarian cancer or colorectal cancer. These genetic tests are recommended for men who are determined through genetic counseling to be at potential risk for hereditary cancer: