Decipher RP Results
Decipher Radical Prostatectomy (RP) is a tissue based prostate cancer marker (PCM) that helps the high-risk patient and their healthcare provider understand if they may need additional treatment following radical prostatectomy.
The Decipher RP test was designed for individuals with high risk features following RP. This includes patients who have positive surgical margins, extraprostatic extension, seminal vesicle invasion, bladder neck invasion, or a PSA rise after RP.
The test looks at the activation of 22 RNA biomarkers (using specialized lab tests using your prostate cancer positive tissue) associated with metastatic progression. These markers review your prostate cancer tissue and evaluate your cancers cell cycle progression, immune system activity and response, androgen signaling pathways, metabolism, and angiogenesis potential (cancer cell blood vessel formation).
Patient Sample Report
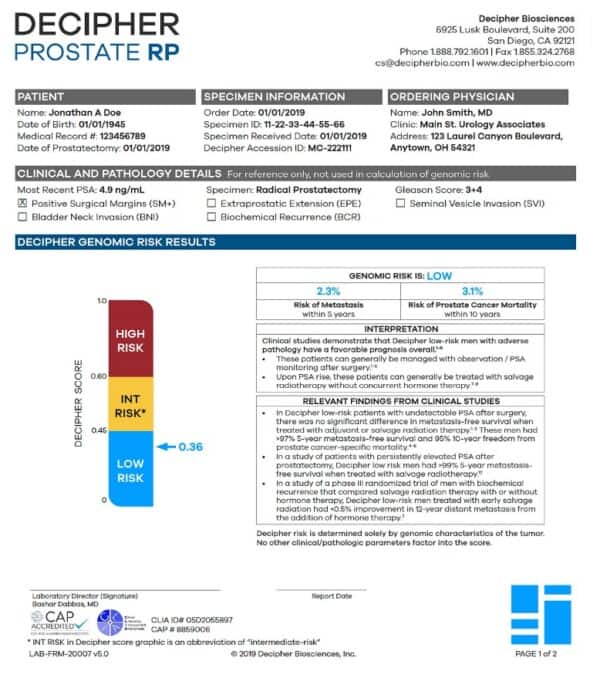
Clinical Details:
This area describes the clinical details associated with your prostate cancer. This information is gathered from your pathology report and is not NOT used to generate your Decipher result.
Decipher Score (Meter):
This section is a visual representation for the overall result of the risk classification for the highest grade cancer that was sampled after your prostate was removed.
This section also describes the overall risk result of your Decipher test. Generally, the lower the Decipher Score (0 being lowest risk to 1 being highest risk) the lower the risk of metastatic spread. This score, as well as your risk percent likelihood (described below) may help your doctor decide to initiate treatment after surgery to reduce the risk of metastases such as hormone deprivation therapy, and/or external beam radiation.
5 Year Metastasis:
This represents your overall risk of having prostate cancer that has spread to other areas, most commonly bone. In this example, 2.3% likelihood means that, if the patient underwent radical prostatectomy, there would be a 2.3% chance the patient may develop metastasis within 5 years. The higher the percentage, the greater the risk.
10 Year Prostate Cancer Specific Mortality:
This represents your overall risk of prostate cancer specific death after 10 years based on the genomic characteristics of your prostate cancer. In this example 3.1% likelihood means that, if the patient underwent a radical prostatectomy, there would be a 3.1% chance the patient may die from prostate cancer at 10 years. The higher the percentage, the greater the risk. This score does not reflect your overall risk of dying of other causes.
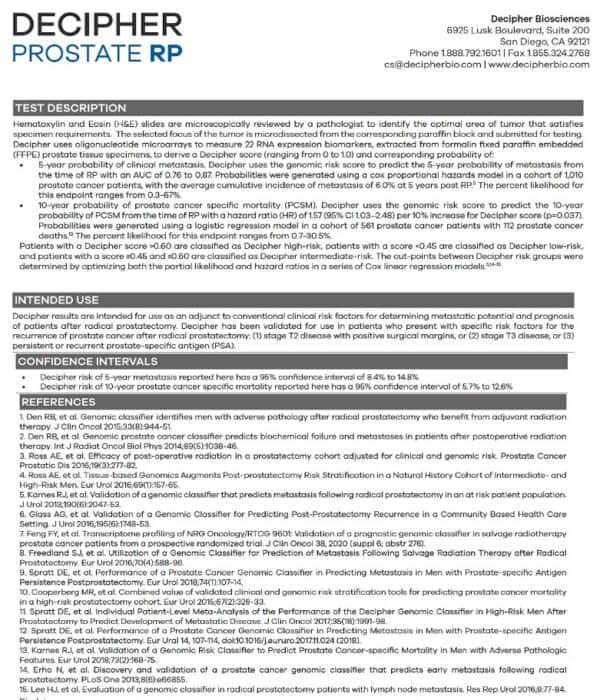
Test Description:
This section describes how the Decipher test works. Essentially, a panel of molecular biomarkers specific to prostate cancer progression and metastasis, represented by multiple biological pathways, are examined from the tumor tissue to determine your individual Decipher Score.
Intended Use:
This section describes how the Decipher Test was intended to be used as a decision-making tool between a patient and their physician, and the type of patient who would benefit most from the test.