Prostate Cancer Screening Saves Lives
Regular PSA screening coupled with biomarker testing for men with elevated levels identifies cancer in early stages when survival rates are 100%!
By E. David Crawford, MD
Men today are more likely to be diagnosed with advanced prostate cancer than a decade ago, with double the number being diagnosed after the cancer has already spread to other parts of the body.
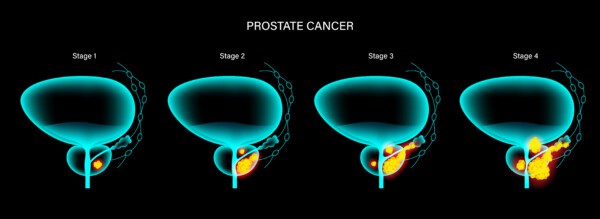
Being diagnosed with advanced-stage prostate cancer significantly increases your risk of dying from the cancer. When prostate cancer is detected early while still confined to the prostate, men have a 5-year survival rate of 100%. However, that number drops to 34% if the cancer is found after it has spread outside the prostate, according to the National Cancer Institute .
We now have the tools to diagnose prostate cancer at its earliest and most treatable stages while minimizing the risks of unnecessary biopsies and treatment. Unfortunately, there is a lot of confusion about prostate cancer screening and so many men are not being evaluated. In this blog, I will outline why and how to be screened for prostate cancer.
The bottom line is this: If you are over 50, you should get a PSA (prostate-specific antigen) screening blood test. (Men with associated risk factors, including a family history of prostate cancer, ethnicity and genetic changes, should start PSA testing earlier.) If your PSA result is abnormal (above 1.5 ng/mL), you should ask your healthcare provider for prostate cancer biomarker testing. These new molecular tests can help determine next steps, including whether or not you should have a prostate biopsy.
Lack of PSA Testing Puts Men at Risk
Beginning in 2008, the US Preventive Services Task Force (USPSTF) stopped recommending the routine use of PSA testing, saying that the potential harm outweighed the benefit. Before the USPSTF decision, the rate of prostate cancer deaths had been steadily declining for 20 years.
Since the task force’s downgrading, the rate of PSA testing has dropped while the rate of advanced-stage prostate cancer diagnoses has increased 4-5% annually, according to the American Cancer Society’s 2023 Cancer Statistics report.
The PSA is the most common test to screen for prostate cancer. Prior to 2008, primary care providers (PCPs) would give nearly every man over 50 an annual PSA test. If you had an elevated PSA level — usually along with an enlarged prostate — you were likely to be referred for a prostate biopsy.
However, an elevated PSA level can be due to a non-cancerous condition or it could be caused by prostate cancer that is very slow growing. Because there were no other tests available at that time, many men who either didn’t have cancer or whose cancer didn’t need to be treated experienced negative effects of unnecessary biopsies and/or prostate cancer treatment. The USPSTF found that up to 50% of men with elevated PSAs were overtreated at the time which led to its recommendations against routine PSA screenings.
The good news is that we now have more accurate tests that can be used along with the PSA test to help us find prostate cancer early and help us determine the right treatment while avoiding treating men who don’t need it. These new tests look for biological markers, also called prostate cancer markers (PCM), which are molecules found in blood, other body fluids, or tissues that are signs of disease.
Should I get a PSA test?
Due to the USPSTF guidelines and different guidelines from various medical organization, many PCPs no longer order PSA tests. However, many prostate cancer experts, including myself, highly recommend that men get regular PSA testing.
You may need to ask for this simple blood test, and don’t be afraid to keep asking. I have had to ask my PCP time and time again for the PSA test—and I work in this field!
Men who are at average risk of developing prostate cancer should start PSA testing at age 50 or older. Men who are at higher risk because of a family history should start at age 45, and Black men should consider screening as early as age 40 years due to higher rates of prostate cancer in this population.
What should I do if my PSA is high?
The PSA test is a simple and inexpensive way to monitor for the possibility of prostate cancer. Notice that I said “possibility.” On its own, the PSA is not a reliable indicator of the need for a prostate biopsy — that’s what led to the problems 20 years ago.
If you have an elevated PSA, you should not immediately get a prostate biopsy. Instead, you should ask your provider for PCM testing. Your provider may not be familiar with these tests, so you might need to push for them.
Biomarker testing provides additional information for you and your provider to consider before taking action. PCM tests can tell you:
- whether your elevated PSA is due to cancer or a benign condition, such as benign prostatic hyperplasia (BPH)
- the likelihood that aggressive prostate cancer will be found through a biopsy
- if cancer is present, how receptive it will be to various types of treatment
- if you have a genetic mutation that puts you at higher risk of developing prostate cancer
A study published in Prostate Cancer and Prostatic Diseases found that when physicians utilized the Prostate Health Index (phi) test for men with a PSA of 4.0-10.0 ng/mL, results reduced unnecessary biopsies by nearly half.
6 Steps to Detecting Prostate Cancer Early
Diagnosing malignant prostate cancer as early as possible gives men the best shot at a cure. Men whose prostate cancer is diagnosed while it is still in the prostate have a 5-year survival rate of 100%! If you are not diagnosed until the cancer has spread, the survival rate falls to 34%.
Here is what you should do to increase your chances of detecting prostate cancer at its earliest stages:
- Know your risk of developing prostate cancer. If you have a family history of breast, colon, ovarian, pancreatic or prostate cancer, you may have a genetic mutation that puts you at higher risk. Other significant risk factors are age and race. Lifestyle also plays a role.
- If you are 50 or older without any known risk factors, ask for PSA testing at your annual physical. If you are African American, talk to your PCP about starting screening at age 40. If you have another risk factor, consider starting PSA screenings at age 45 or younger.
- If your PCP recommends against PSA testing, ask whether they know about and use biomarker testing that can help refine the findings of a PSA test. Or ask them to consider giving you a 4Kscore test in place of a PSA test.
- If your PSA is less than 1.5 ng/mL, which will be the case for 8 out of 10 men, talk to your PCP about re-screening in 5 years.
- If your PSA is 1.5 ng/mL or higher, your PCP will likely conduct a digital rectal exam (DRE) to assess the size of your prostate and any suspicious nodules. You and your PCP should consider prostate biomarker tests for additional insights and/or repeating the PSA test in 6 months.
- Based on the combined results of your elevated PSA score, DRE, and biomarker testing, discuss prostate biopsy with your provider. Having more than one of these factors increases the likelihood of prostate cancer.
E. David Crawford, MD, is the founder of PCMarkers.com and a board-certified urologist who has dedicated his career to prostate cancer awareness, research, and treatment. Men’s Health Magazine has recognized Dr. Crawford as one of the top 20 urologists in the country. He is currently a Professor of Urology at the University of California San Diego School of Medicine and sees patients at UC San Diego Health.